Coeliac Disease and gluten sensitivity
How common is coeliac disease?
- Population screening has shown that 1:85 people have coeliac disease. Many people are unaware of the diagnosis. Symptoms may be severe (such as diarrhoea, bloating, weight loss) but the condition can also be present with no gut symptoms
What is gluten sensitivity (where coeliac disease has been excluded or appears unlikely)
- There is a significant proportion of people who feel better on a gluten-free diet but who do not have coeliac disease (termed non-coeliac gluten sensitivity). The popularity of a gluten-free diet can be partly attributed to "fashion" but there is no doubt that genuine benefits to wellbeing are behind the increased popularity of the diet
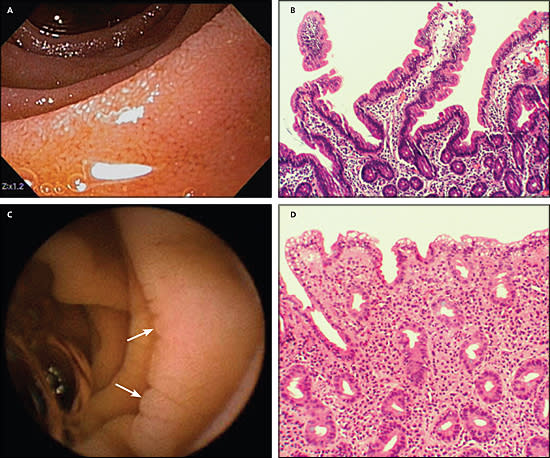
- The challenge to the medical profession is how to understand this benefit and to try to understand the mechanism for this benefit. Coeliac disease is a well understood immune-based condition with a well-defined change in the lining of the small bowel but gluten sensitivity has no agreed definition or tests
- There may be a genetic basis - people with the susceptibility gene DQ2 may have more gut symptoms and respond to a gluten-free diet. Recent studies have cast doubt on this idea - the benefit of a gluten-free diet for abdominal symptoms may be due to reduction in fermentable carbohydrates and this benefit is the same regardless of DQ2 status.
- The interpretation of various antibody tests is debated. Tissue transglutaminase (discussed below) suggests coeliac disease. Other less accurate tests probably simply give false positives and are not predictive of a response to a gluten-free diet
- Hopefully more research will clarify this issue
What is the benefit of diagnosing the mild cases of coeliac disease?
- With better tests and greater awareness amongst doctors and also in the community there are more people who are being diagnosed with coeliac disease. Many of these people could be considered to have mild disease.
- Most people are pleased with the diagnosis and feel the benefit of the diet. However we also need to consider whether everybody with a positive test found by screening benefits from the diet
- In a large UK health survey of individuals aged 45-75 years 1.2% had positive endomysial antibodies i.e a diagnosis of coeliac disease.
- There was no difference between subjects who were antibody positive or antibody negative for a wide range of indicators that were used to measure health and general well-being.
- The only significant difference was a higher proportion of antibody positive subjects who had anaemia (16% compared with 4%).
- There was a trend towards lower bone density in those subjects who were antibody positive
- This study confirms the importance of checking for coeliac disease if there is iron deficiency (+/- anaemia) without any other obvious cause.
- It is perhaps helpful to use an “iceberg” analogy for coeliac disease with overt severe disease at the top and mild or silent disease forming the majority below sea level.
- We are diagnosing a lot more people with mild coeliac disease. Also some with "silent" disease.
- All patients with coeliac disease should attempt to be as gluten-free as possible but it is tempting to be less strict with less severe disease. The reasons to be as careful as possible are discussed below
Treatment of coeliac disease
- The only treatment is a gluten-free diet.
- There is usually a rapid improvement in symptoms over a few weeks.
- Continued improvement can occur over the first 6-12 months.
- If there is not any improvement specialist review is required.
- Adherence to a gluten-free diet is easier when there is a clear correlation between gluten exposure and abdominal symptoms. This is not always the case. Some people do not observe any direct relationship between inadvertent gluten exposure and symptoms.
- Adherence to the diet has become easier because of a wide range of commercially available gluten-free foods and the mandatory labelling of foods for gluten content.
- Helpful advice is available thorough dieticians and through the Coeliac Society of NZ.
- Dietary supplements are not usually required except during the first 6-12 months if significant nutritional deficiencies are identified.
- Prompt replacement of vitamin D (if low serum vitamin D) is appropriate.
What are the advantages of gluten-free diet when there are no or few abdominal symptoms?
There are four main arguments for a gluten-free diet in this situation.
- You may be surprised by how much better you feel!!
- That is, there has been an acceptance of a decreased level of well-being and energy levels as part of normality.
- It is also common to have accepted abdominal bloating and flatulence as normal.
- Any nutritional deficiency is highly likely to correct on a gluten-free diet without the need for supplements. This includes nutrients that are easily measured (iron, folate, B12, calcium, vitamin D) AND also other nutrients that may be important for well being (but are not easily measured).
- Osteoporosis is a definite risk with untreated coeliac disease although the fracture risk may not be that large.
- Bone density does improve significantly on a gluten-free diet.
- There is an increased risk of some cancers with untreated coeliac disease.
- This includes two rare cancers - small bowel lymphoma and small bowel adenocarcinoma.
- This also includes a slightly increased risk for other more common abdominal cancers (stomach / oesophagus / pancreas /bowel). However, the overall cancer risk may not be different (or only marginally elevated).
- For example some studies show that risk of breast cancer is reduced in coeliac disease (so there are "swings and roundabouts").
- The risk is most apparent with more severe disease (ie. significant gastrointestinal symptoms) and with later age of diagnosis (more than 50 years).
- The important fact is that the risk is virtually eliminated with a gluten-free diet.
- There is an increased risk of auto-immune diseases (type 1 diabetes, thyroid disease, Sjogrens disease).
- It is not known if a gluten-free diet protects against getting an auto-immune disease but in theory this is a likely effect if the disease is diagnosed as a young adult.
- There is a skin disease associated with coeliac disease called dermatitis herpatiformis. There are itchy raised red spots on the back, buttock and thighs - sometimes small blisters. This responds to a gluten-free diet but may take several months or even years to completely respond. A skin biopsy can be useful to accurately diagnose the problem.

Comments